Disc Prolapse is a common medical condition, which a person experiences when body structures designed to hold internal organs in place weaken or stretch, causing them to eventually “fall out of place”. This term can be used to define misalignment of the heart valves (mitral valve prolapse), the protrusion of the rectum (rectal prolapse), or even spinal disc herniation (lumbar disc prolapse).
In this article, we will be exploring answers to the question ‘What is a Disc Prolapse?’. The causes of disc prolapse, prolapsed disc symptoms, the severity of the pain and seriousness of a prolapsed disc will be all covered.
Most importantly, based on the statistics, you will also learn about how long it does take to heal recover from a prolapsed disc. And, all the treatment options for a prolapsed disc.
Tip: Terms disc protrusion, disc herniation and disc bulging are commonly used, and they have very similar meanings but explain different stages of intervertebral disc deformation. Some of those conditions/terms we have previously covered.
With no further due, let’s dig further into what is a prolapsed disc means.
A prolapsed disc in the lower back
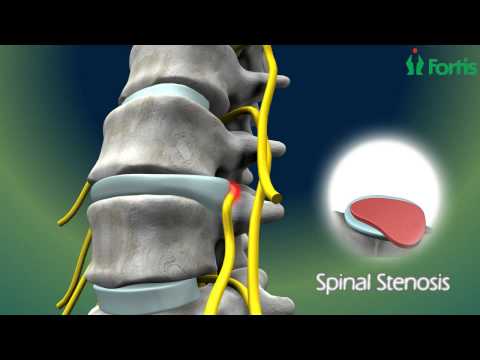
Lumbar disc prolapse (or lumber slipped disc), accounts for less than 5% of all lower back pains but considered one of the most common causes of sciatica pain.
In sciatica, pressure on one or several nerves in the vicinity of the sciatic nerve leads to lower back pain. In addition, a patient may also experience tingling sensation and numbness, which is referred to as “pins and needles” feeling. Lower body muscle weakness and loss of elasticity are also common as sciatica left untreated.
Tip: If you feel tired and weak most of the time with no understandable reason that could be a sign of chronic fatigue syndrome, where you may be eligible for a disability claim.
Lumbar disc herniation occurs when the fibrous ring of a vertebral disc ruptures opening (or cracking), allowing the nucleus pulpous to escape. Intervertebral discs between the relatively flexible lumbar vertebrae are particularly vulnerable to prolapse as this area of the spine bear considerable weight and support a wide range of motion.
In most instances, symptoms rise with a disc prolapse are managed and reversed with conservative or non-surgical treatments (for example, pain killers, rest, physiotherapy or exercise). Surgery would be necessary in case the pain interfere with lifestyle, to provide faster pain relief and avoid disability in the minority of patients whose recovery is unacceptably slow.
What causes disc prolapse?
Transmission of the serious impact through the spine is due to the falling
is a common cause of disc prolapse. For example, falling on your buttocks or falling from a height. If the force is strong enough, a vertebra (bone) may fracture or an inter vertebral disc may rupture.
Leaning forward posture puts substantial pressure on the inter vertebral discs too. If you bend and attempt to lift a very heavy object, this force may cause a disc to rupture.
Intervertebral discs may also rupture as a result of a weakening of the disc’s outer fibers. This usually occurs due to repetitive minor injuries that accumulate over time. This damage can occur with aging, hereditary factors, work-related or recreational activities. Well, there’s no such reason for the occurring of this process. But in some cases, a simple lift, twist or bend in a way can cause enough pressure on the disc which results in rupture its weakened outer fibers.
Tip: Pressure on a disc is different from pressure on blood vessels. Coconut oil, garlic oil and krill oil could help to lower blood pressure depending on the stage of hypertension.
What are the prolapsed disc symptoms?
You may have a prolapsed herniated disc anywhere in your spine, from the neck to your lower back. The commonly affected area is the lower back for slipped discs.
Your spinal cord is an intricate network of nerves and blood vessels. A herniated disc can put extra strain on the nerves and muscles around it.
Some major prodrome of a prolapsed disc at an early stage are below.
- The loss of bladder or bowels control,
- changes in the sex organ space and erectile dysfunction (impotence) in men
- lack of sensation/numbness, pricking or tingling in one’s arm or leg
- Pain in the shoulder bone or the glutes
- severe pain in arm and/or leg
- The nerves that have been affected are due to position of the symptoms
- Symptoms help determine your diagnosis
- Weakness concerning one or both arms or legs
Tip: Different parts of the leg experience pain due to different causes. Here are the causes for groin pain, thigh pain, back of the leg pain, knee pain, calf pain and foot pain. If the back pain appears only at night, that can be due to diabetes.
Tip: Similarly, causes of lower back pain can be different from upper back pain.
How painful is a prolapsed disc?
When lumber disc prolapsed or slipped disc, it causes severe lower back pain. The disc frequently presses on a nerve root which can cause pain and other symptoms in a leg. In most cases, the symptoms ease off progressively over several weeks.
If there are solutions to the underlying causes of the symptoms occurring, they need to be addressed as soon as possible.
Painkillers at an urgent call can be helpful. Spinal manipulation is a part of manual therapy can be a satisfactory remedy. Physical management can be a second option before moving to surgery. Still, pain perseveres surgery can be carried out with doctors guidance.
In addition to back pain, you may feel pain below your knee as far as your calf or foot.
Nerve root pain can be a dreadful discomforting, more than the back pain. It is mostly misinterpreted by searing pain.
The sciatic nerve is the most affected with a prolapsed disc. The period sciatica means nerve root pain of the sciatic nerve. Enormous tiny nerves make up the sciatic nerve which directionally comes from the spinal cord in the bottom-most pain (lower back). The pain is to feel along the buttock descending in the back of the leg even running down to toes or foot.
Tip: Here are the proven remedies to cure sciatica.
Tip: If you are not sure about the reason for your back pain, make sure to differentiate the back pain from kidney pain.
Is a prolapsed disc serious?
The seriousness of disc herniation or prolapsed disc can be made by observation of symptoms and physical examination, but it can also be confirmed by tests such as computed tomography (CT) or magnetic resonance imaging (MRI), which serve to evaluate the disc, its thickness, the exact location of the hernia and what kind of hernia one has.
The x-ray examination may not show the hernia clearly, but in most instances, an x-ray image may be sufficient to show spinal alignment and vertebrae integrity or destruction, so sometimes the doctor initially requests the x-ray and with the result of this, requests resonance or tomography to assess severity.
The damaging to the disc hernias or bulged will cause to surpass some basic treatment like physical training, Pilates, osteopathy or medical procedure. If no such improvements are being shown in the symptoms, surgery is the last obtainable possibility to treat, especially if it exceeds longer than six months.
Tip: People with chronic pain are prone to depression, anxiety and stress. They may struggle to sleep through the night.
How long does it take to recover from a prolapsed disc?
Sometimes it’s the vice versa of the case. The agony from a prolapsed herniated disc will get progressive in a couple of days or maybe weeks.
Most of the time, all this will happen due to the conscious attitude towards the symptom. Like taking medication on time, heat/ice therapy, or confining some of the activities. The remedies could be in the form of pain relief, non-steroidal anti-inflammatory pills and relaxants medication.
Approximately half of all patients experience a prolapsed disc will improve within 10 days, but the majority of the patients take up 4-6 weeks to recover. However, less than 10% of people will not recover even by the 12th week, where they need to consider intensive physiotherapy or surgery to improve the symptoms.
Tip: If the disc prolapse is due to an injury, stick with one of the best wound dressings to speed up wound healing.
What is the treatment for a prolapsed disc?
The first treatment for a prolapsed herniated disc is a short rest period with analgesic medications, and for quicker recovery should be followed by physical therapy. People are seen to have a faster recovery by simply following these treatments and going back to their normal activities.
Few people will need more treatment, which may include steroid injections or surgery.
Medicines
Medicines may help reduce pain. Your doctor may prescribe:
Non-steroidal anti-inflammatory drugs can be helpful as long-term pain control.
Opioids in case of severe pain that does not respond to anti-inflammatory drugs.
Muscle relaxants to control back muscle spasms.
Lifestyle changes
Diet and exercise are crucial for improving back pain in overweight patients.
Physical therapy is important for almost all people with a prolapsed herniated disc. Therapists teach how to properly lift objects, dress, walk, and perform other activities. They work to strengthen the muscles that help support the spine. You will also learn to increase the flexibility of your spine and legs.
Home care may include:
- It may be advisable to reduce activity in the early days. Then slowly resume your normal activities.
- Avoid lifting too much weight or twisting your back for the first six weeks after the onset of pain.
- After two to three weeks, exercise again gradually.
Temporary pain relief
Steroid injections and anti-inflammatory medications are used after numbing the epidural space of the spine, this is done due to the help of x-ray fluoroscopy, and an injection is thrust.
The painful areas are being injected to reduce the swelling and inflammation of the nerves. Although the procedure provides only temporary relief, most of the patients are satisfied by the ease. Repetitively, injections are used to extend the result in full fledge although the ease varies either for months or years.
Surgery
Surgery is the last option left if no such improvements are shown following non-surgical treatment.
In some cases, the pain becomes so severe that the symptoms can be harmful. In less extreme cases, 9 out of 10 patients are satisfied by not proceeding to the surgery. The main purpose of the surgery is only to remove the prolapsed section of the disc and discharge the pressure effectuate on nerves.
No doubt this has been an intense situation, but it also follows a risk from surgery. Your consulting doctor should explain the indications for fors and againsts the operation.
Although it has not still figured whether surgery is the only option with successful results or its better to wait for the results with other medication, the latest research implies that surgery is better in the quick-term but makes no exception in the extended term.
The implementation of the surgery does not vividly modify the volume of suffering on the effect of someone’s lives.
Let’s look into the 4 key types of surgeries for disc prolapse repair.
1. Anterior cervical discectomy & fusion (ACDF)
Does the surgical procedure involve a hole made in the neck? In this Anterior cervical discectomy and fusion surgery, the neck muscles are transposed to reveal bony vertebra and disc. The damaged disc is removed that create a push on the nerve.
Herniated material is removed whereas space is filled by a bone transplant to create a coalition. With the help of a coalition, two or more bones are joined. A proper bone is located with the help of the grafting process combine with the vertebra. To brace the stability fusion, metal plates or screws are likely used.
2. Total Disc Replacement (TDR)
During an anterior discectomy, a conveyable tool that simulates a disc’s movement is inserted into a broken joint space.
The artificial discs maintain a motion, whereby fusion reduces motion. They are as usual made up of metallic and plastics also used for the hip and knee implants technique.
The major difference between the ACDF and cervical disc replacement is the perseverance motion that avoids adjacent level disease.
3. Micro endoscopic discectomy
A hole is being made in the nape of the neck to expand the tunnel to the vertebra. Tiny tubes as dilators square measure are practice in which a piece of a bone is eliminated to disclose the nerve root and discs. Then the surgeon uses a magnifier to get rid of the rupture disc.
However, the micro endoscopic discectomy
procedure is less painful for the muscles than conventional discectomy. It is also likely to cause less serious damage to the nerves.
4. Posterior cervical discectomy
In a posterior cervical discectomy, 1 to 2 inches of gash is made at the back of the neck. Intending to reveal the bony vertebra, the spinal muscles are dissected to reach the broken disc.
To achieve the nerve root space, a bony arch or lamina is removed from a vertebra. The piece of the burst disc or safety disc the stresses the nerves spinal is removed. The existence of the nerve in the spaces is expanded to limit the future, causing pinching.
Can prolapsed disc get worse?
Most people with a prolapsed or herniated disc get better in about four to six weeks, or sometimes it might take longer. But if someone is still suffering from pain or numbness after four to six weeks, there’s a chance for the problem to get worse. In that case, you need to consult with your doctor as soon as possible to explore other treatment options such as surgery.
Tip: Thumper massager or a foot and calf massager could help with pain-relieving.








0 Comments