In this article on Type 2 Diabetes Complications Timeline, we are going to explore about 12 possible complications of Type 2 Diabetes and the timelines a person with poorly controlled diabetes likely to come across those complications.
Before anything, let’s recall some basics about diabetes.
What is Diabetes?
Diabetes mellitus is one of the leading causes of death and other health complications worldwide. According to the World Health Organization, the number of people diagnosed with diabetes increased from 108 million in the year 1980 to 422 million in 2014.
This number is anticipated to hit a billion in the near future. It also recorded that about 1.6 million deaths were directly linked to diabetes as of 2016, thus, making diabetes the seventh leading cause of death.
Diabetes is a chronic disease that ultimately has an impact on the blood glucose level. Unlike what most people think that ‘it occurs when one takes sugary foods’ (This is a Myth!); it is usually caused by a disorder of the pancreas whereby the pancreas is unable to produce enough insulin. It is also caused when the body cells cannot effectively use the insulin produced by the pancreas. In some cases of diabetes, it is a combination of both. In a case where any of this happens, the result is that the body is unable to take in glucose from the blood into the cells and this leads to high levels of glucose in the blood (a condition termed ‘hyperglycaemia’).
Diabetes is of two major types; the Type 1 and Type 2.
What is Type 1?
Type 1 diabetes is an autoimmune condition whereby your body’s immune system mistakenly attacks its own cells – the beta cells of the pancreas that are responsible for producing insulin. The damage, in this case, is permanent.
Type 1 diabetes often occurs from childhood and is thus called ‘juvenile-onset diabetes’.
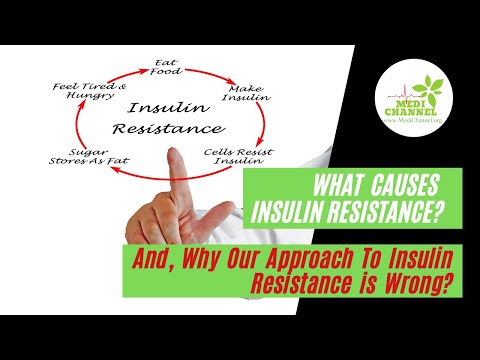
What is Type 2?
Type 2 diabetes, on the other hand, occurs as resistance to insulin. That is to say, the body is unable to effectively use insulin.
It is the most common type of diabetes in the world; more than 95% of diabetic adults are in this category. It is also termed ‘adult-onset diabetes’.
Diabetes type 2 is seen as a mild one when compared to type 1; however, it has been indicated to cause certain major health complications with time.
Most people tend to ignore type 2 diabetes, especially at the early stage when it seems they don’t feel the impact but in the long run, if not treated, it could affect major organs such as the nerves, blood vessels, heart, kidneys and even eyes.
As noted above, in this article, we would delve deeper into the complications that could arise from type 2 diabetes and organs affected.
Listed below are some of the key organs and body systems you should keep an eye on for any signs of diabetes-related complications.
1. Diabetes Effect on Heart and Blood Vessels
The functioning of the heart and blood vessels are interlinked. Type 2 diabetes affects blood vessels most especially the large blood vessels.
Heart Diseases Heart Attack and Stroke
In fact, diabetic patients have higher chances of developing heart disease, heart attacks and stroke.
One would ask, “What exactly is the link between diabetes, heart diseases and stroke?” The fact is that people with diabetes are mostly prone to other health conditions and have higher chances of developing other risk factors, which ultimately increases their chances of heart diseases or stroke.
High Cholesterol and Diabetes
Some of those risk factors include high cholesterol level and high blood pressure.
Diabetes is a chronic health condition, and over time, the high blood glucose could induce damage to your blood vessels as well as the nerves that supply your blood vessels and heart.
Young people with diabetes have a higher tendency of developing heart diseases at a tender age when compared to non-diabetic individuals.
The good news, nevertheless, is that you can manage your health condition and thus reduce your chances of developing heart diseases and stroke.
Tip: ResPerate is a modern-day blood pressure-lowering technology.
Risk Factors for Heart Diseases and Stroke in Diabetics
Risk factors that could predispose you to stroke and heart diseases or cardiovascular disease as a diabetic patient include the below.
- Smoking
- Abnormally high cholesterol levels
- High blood pressure
- Belly fat and obesity
- A family history
of heart diseases
Always monitor your blood pressure level and ask your physician about your cholesterol numbers.
If you have been smoking, then it is time you call it quits.
2. Diabetes Effect on Body Weight
Whether you have diabetes or not, obesity generally poses serious health complications.
Overweight and Obesity
Being overweight would not only increase your risk for many health complications as a diabetic patient, it will also interfere with your ability to manage your health condition.
The Link with Diabetes
As much as it is believed that obesity promotes type 2 diabetes, diabetes also promotes or increases the chances of gaining weight. Both diseases are highly interconnected.
Diabetic people usually undergo a type of hormone therapy called Insulin Therapy, and this causes people to gain weight. Insulin is a hormone that regulates the blood sugar level; however, it can cause weight gain when it causes the cells (mostly the cells of the muscles, fat and liver) to absorb much glucose than the body needs at that point in time. When the cells are unable to use the glucose to generate energy, at that point, they are being converted into fat for future use. As the body continues storing glucose in the form of fat, such individual gains more and more weight.
According to an estimate made by the World Health Organization, about 90% of people diagnosed with type 2 diabetes are either obese or overweight. No doubt reducing the excess body fat can help in diabetes management.
3. Diabetes Effect on Kidney
How Exactly does Diabetes Affect Your Kidneys?
Glomerular nephritis and glomerulosclerosis are both medical conditions related to kidney problems.
Glomerulonephritis
Glomerular nephritis also called glomerulonephritis is inflammation of the glomeruli (tiny filters in the kidney that act to eliminate the excess electrolytes, fluid and toxic waste from the bloodstream before passing them into the urine).
Glomerulosclerosis
Glomerulosclerosis, on the other hand, is a condition in which the glomeruli get scarred and hardened.
Both conditions interfere with the normal functioning of the glomeruli, which is to remove waste products and urea from the bloodstream through the urine.
Diabetic Neuropathy
Prolonged high blood glucose as in the case of diabetes can cause damage to the kidneys and cause a condition known as diabetic neuropathy.
Kidney Failure
Diabetes damages the microvessels (small blood vessels) that supply blood to the kidneys. Over a few decades, this could lead to kidney failure, which starts manifesting as an inability of the kidney to filter blood efficiently. The body starts retaining more amount of salt and water. The symptoms of this are weight gain, ankle swelling and build-up of toxic materials in the blood.
Tip: Chinen Salt is a better option for diabetics compared to regular salts.
Urine Retention Leading to Urinary Tract Infections
Diabetes also causes damage to the nerve cells. Nerve cells that supply the bladder are not exempted from this damage, and when they get affected, it can lead to difficulty in emptying the bladder. There can be a build-up of pressure within the bladder which can in turn cause injuries to the kidneys. In addition, urine retention in the bladder can also cause bacterial growth and ultimately infection.
According to statistics, about 30% of Type 1 diabetic patients and 10%-40% of Type 2 diabetic patients will eventually suffer from kidney failure.
4. Diabetes Effect on Eyes
Diabetes causes an array of eye conditions called ‘diabetic eye disease’. Diabetic eye diseases are a group of eye conditions that can easily be developed by people with diabetes. They include diabetic retinopathy, glaucoma, cataract and diabetic macular oedema.
Diabetic Retinopathy
Diabetic retinopathy is a diabetic eye disease that is caused by damage to the blood vessels in the retina. The macula of the eye is an area located in the centre retina that provides us with accurate and central vision.
Maculopathy
Maculopathy is a pathological condition of the macula.
Cataract
A cataract is an eye condition that is characterized by clouding of the eye’s natural and normally clear lens.
Yes, high blood sugar can cause all the above-mentioned eye conditions.
Blindness
According to research articles, diabetes is the major cause of blindness in adults between ages 20 and 74. Also, each of the eye conditions classified under diabetic eye diseases has the potential of causing severe loss of vision.
You may not easily detect some of them, such as the diabetic retinopathy, early. That is more reason why it is crucial that every diabetic individual makes regular visits to the eye doctor (Optometrist or Ophthalmologist), so that any case of such can be detected and treated early.
5. Diabetes Effect on Nerves
Diabetic people are also prone to nerve damage.
Diabetic Neuropathy
Nerve damage that results from the build-up of glucose in the blood is known as diabetic neuropathy.
There are different types of nerve damage, each with its own symptom. Their common symptoms include pain and numbness in the limbs as well as abnormal functioning of the internal organs.
What is Diabetic Neuropathy?
Any form of nerve damage induced by diabetes is known as diabetic neuropathy.
As you know, diabetes is a chronic health condition characterized by high sugar level in the blood and over time blood sugar as well as fats such as triglycerides build up in the blood. This can result in nerve damage.
Symptoms exhibited by the individual depends on the nerve affected or the type of diabetic neuropathy.
Diabetic neuropathy is of four major types, as noted below.
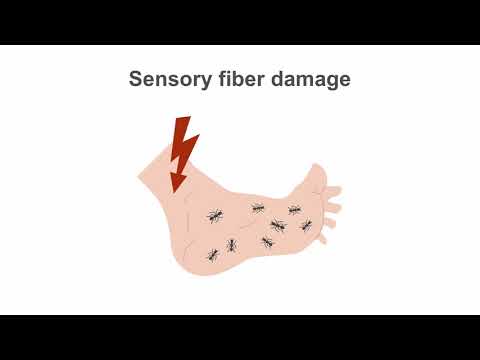
Peripheral Neuropathy (Neuritis)
This is damage to the peripheral nerves and is the most common type of diabetic neuropathy.
It usually affects the lower limbs first, then followed by the upper limbs.
Its symptoms manifest as numbness, stabbing pains, tingling or burning sensation, muscle weaknesses, loss of reflexes and foot problems like an ulcer.
Autonomic Neuropathy
The autonomic nerve system (ANS) is that part of the nervous system that controls the heart, internal organs of the abdominal and pelvic regions as well as the eyes. Damage to nerves in these areas can lead to bladder problems,
Ø constipation,
Ø difficulty in swallowing,
Ø inability to control body temperature,
Ø decreased sexual response and
Ø sweating less or excessively.
Mononeuropathy
Mononeuropathy is damage to a specific nerve located in the face, the centre of the body or the legs.
It is usually accompanied by pain in the abdomen, pelvis, foot or anterior part of the thigh.
Diabetic Amyotrophy
Diabetic amyotrophy affects certain nerves located in the thighs, hips, legs and gluteus (buttocks). Diabetic amyotrophy is quite common in people with type 2 diabetes.
Symptoms could present as weakness of the thigh muscles, pain in the hip, thigh and gluteus, abdominal swelling and weight loss.
Tip: Check it out these Pressure Ulcer Prevention Devices.
6. Diabetes Effect on Extremities
Diabetic Foot
Diabetic people tend to have a high tendency to develop problems with the extremities, especially the lower extremity as in the case of foot problem known as ‘diabetic foot‘. This is due to prolonged periods of high sugar in the blood. Foot problems often occur as a result of damage to the peripheral nerves (peripheral neuropathy).
The symptoms accompanying this include burning or tingling sensation and weakness in the feet. There is numbness and decreased sensation in the feet, which can, in turn, increase the risk of cuts, blisters, sores and foot infections.
Numbness in the Feet
With numbness in the feet, it may be difficult for the diabetic individual to feel the soreness, irritation or infection in the feet.
Tip: Did you know Diabetic Socks and Stockings can help your fight with the diabetic foot?
Gangrene Requiring Amputation
When left untreated foot infections can cause ulcerations and even development of gangrene. With the development of gangrene (a dead tissue condition in which tissues in the lower extremity rotten as a result of insufficient or lack of blood supply) amputation of the affected foot may be inevitable.
Asides the nerves, as noted before, diabetes can also affect the blood vessels supplying the lower and upper limbs leading to changes in those blood vessels. Presence of fatty deposits could block the blood vessels (peripheral vascular disease) those blocking blood flow to both limbs. The result is pain, infection, slow wound healing and in serious cases – amputation.
7. Diabetes Effect on Bones
With diabetes, you are at higher risk of developing bone and joint disorders. Even though their cause may seem idiopathic (without an identifiable cause), is that certain factors such as diabetic neuropathy, obesity and arterial diseases can contribute to bone conditions.
Some of the bone and joint problems associated with diabetes include below.
Osteopenia
This is bone loss, a condition that can easily be predisposed by diabetes.
Here, the body is unable to make new bones as quickly as it does reabsorb the old one. The bones keep wasting and getting thinner and at a point, could eventually lead to osteoporosis (abnormally porous bone).
Charcot Joint – Arthropathy
Also called neuropathic arthropathy, is a condition that occurs when the joint deteriorates as a result of nerve damage. It is a common complication associated with diabetes and usually affects the feet.
The affected joints may become red, warm and swollen with loss of sensation.
Diabetic Hand Syndrome
This is also called diabetic cheiroarthropathy. This is a health disorder in diabetic people that is characterized by thickening of the skin on the hands.
The skin covering the limbs become waxy and eventually leads to restricted movement of the fingers.
8. Diabetes Effect on Immunity
Diabetic people have a high tendency of developing different types of infections which includes infection of the lungs, skin and urinary tract, all due to poor immunity caused by diabetes. These infections affect the transport of glucose into the cells and tissues.
Lung Infections
With diabetes, one is highly susceptible to respiratory tract infection.
Lung infection is usually accompanied by changes in the ciliary epithelial lining. Because people with diabetes have a reduced capability of their antibodies to produce protein antigens, they become more susceptible to pneumococcal infection.
Tuberculosis
There is also a link between diabetes and pulmonary tuberculosis too.
According to a review article published on PubMed about the causes of lower respiratory tract infections in people with diabetes, people with diabetes have 4-5 times greater risk of developing tuberculosis than the non-diabetic people. Malfunctioning of monocytes in diabetic patients may be one of the causes of this.
Skin Infections
Diabetes can affect any part of the body, the skin inclusive.
In fact, skin problems resulting from diabetes are usually the first signs to manifest before other complications arise. Anyone can develop such skin problems, but people with diabetes are at higher risk of developing them. Bacteria or fungus cause most of those infections.
Some other skin infections include diabetic blisters, diabetic dermopathy and eruptive xanthomatosis. The good news if it detected early, most of them can be easily treated.
Urinary Tract Infections (UTIs)
The presence of sugar in the urine does increase the chances of bacterial growth and thus, infection. When your blood glucose levels are not properly managed and controlled, you would be more susceptible to urinary tract infections.
Urinary tract infections can occur anywhere in the urinary tract, which includes the kidneys, bladder, ureters and urethra.
According to data recorded by the American Diabetes Association, 9.4% of Type 2 diabetic people had a urinary tract infection compared to only 5.7% of people without a health history of diabetes.
9. Diabetes Effect on Healing – Slow Wound Healing
With a diabetic condition, your wound could take a longer duration to heal. This further increases the risk of other complications, such as infections and amputations.
The Centres for Disease Control recorded that about 30.3 million people suffer one type of diabetes or the other, and a large percentage of these people suffer from complications resulting from infected wounds.
What is the Effect of Diabetes on Wound Healing?
You might be wondering how and why diabetes affects wound healing.
A study carried out in 2013 explained that there is a correlation between blood sugar and wound healing. The study showed that people undergoing surgery for diabetic wounds had higher chances of healing fully, if they managed their condition well and controlled their blood glucose level at the time of the operation.
Dropped Immunity
A prolonged increase in the blood glucose level can impair the normal functioning of white blood cells which play a central role in conferring immunity to the body system. When the body’s defence system is impaired, the body becomes unable to fight bacteria and to heal wounds.
Poor Blood Circulation
Diabetes also predisposes to poor circulation of blood.
Blood moves slowly making it difficult for sufficient oxygen and nutrients to be supplied to the site of the wound. The resultant effect of this is that the wounds heal slowly or in the worst cases, do not heal at all.
Slow healing of wounds, as well as reduced sensation in that region, increases the risk of infection.
Tip: Learn more about A1c Testing here.
10. Diabetes Can Cause Cancers
A time ago, it was under speculation, but now, researches have confirmed that diabetes and cancers are linked and that diabetes increases an individual’s risk of developing cancer. Research also confirmed that women with diabetes are more affected.
How Does Diabetes Cause Cancer?
The question that should follow suit is “how does diabetes cause or increase the risk of developing cancer?”
And, does diabetes treatments trigger cancer development? Or perhaps, the underlying causes of diabetes also causes cancer.
Now, the mechanism of this correlation is still poorly understood; however, some researchers have argued that high blood glucose levels over a prolonged period could cause damage to an individual’s DNA, thus increasing the risk of developing cancer.
Could Diabetic Medications Increase the Risk of Cancers?
Also, there is a proof (though not definitive) that certain diabetic medications could increase the risk of cancer. For example, research showed that long-acting insulin could increase cancer risk.
However, because, this link between diabetes treatment band cancer, is still not definitive, we advise that people with diabetes should go ahead and treat their condition using the appropriate medications as prescribed by their doctors without the fear of cancer.
As I always say, your doctors’ advice should be what is most important in the management of your specific health condition, but not our generalized opinion.
11. Diabetes Effect on Hearing – Hearing Impairment and Hearing Loss
There is a strong connection between type 2 diabetes and hearing loss. This is one reason why it is crucial that you manage and control your health condition ‘diabetes’, well. When you don’t properly control your blood sugar levels, you are at increased risk of developing hearing loss or hearing impairment.
What does the Research Say about Diabetes and Hearing Impairment?
Researches have shown that hearing loss in people with diabetes is twice as that which occurs in non-diabetic people.
A research study carried out in 2008 also suggested that diabetes could cause hearing loss by damaging the blood vessels and nerves. Even though no distinction was made between those that had type 1 and those that had type 2 diabetes, it was clear that most participants in the study had type 2 diabetes.
What Causes Hearing Loss in People with Type 2 Diabetes?
The exact cause of the hearing loss in diabetic patients is still vague. However, one certainty is that high blood sugar can damage different blood vessels and nerves in the body; the network supplying the ears are not excluded.
Surely, without doubt, damage to the auditory nerves as a result of diabetes could lead to loss of hearing.
12. Diabetes Effect on Sleep – Sleep Apnoea
In clinical research, certain sleep-disordered breathing conditions such as the Obstructive Sleep Apnoea (OSA) have been linked with glucose intolerance as well as insulin resistance.
Sleep Apnoea
Some of the typical symptoms of sleep apnoea include pausing in between breaths while sleeping and loud snoring.
This condition is caused by obstruction of the upper airways.
Diabetes and obesity are major risk factors for sleep apnoea.
Sleep apnoea is common in people with diabetes and has very important clinical consequences such as daytime sleepiness and poor quality of sleep.
Asides that, sleep apnoea also causes low oxygen levels because of the temporary blockage that prevents are from getting to the lungs. This could affect the brain and the heart, as well.
13. Other Complications of Uncontrolled Type 2 Diabetes
Asides the above-mentioned complications that could arise as a result of diabetes, there are some other complications of type two diabetes you should be wary of, though some of them are short-term complications.
Hypoglycemia
Hypoglycemia is a term used to describe an abnormally low blood glucose level.
If you are taking insulin drug to control your glucose, take it with caution and ensure that you follow the dosage prescribed by your doctor, as if not, your blood glucose can drop too much. This condition can be equally life-threatening.
Hypoglycemia can also be caused by other medications such as aspirin and excessive intake of alcohol (by a diabetic patient).
Some of the signs and symptoms of hypoglycemia include:
§ sweating
§ anxiety
§ increased or rapid heartbeat
§ a numb sensation in the toes, fingers and lips
§ sleepiness
§ headache
§ slurred speech
§ confusion
If you take insulin medications, then you might as well carry glucagon along with you always as it is possible for one to get unconscious or unresponsive as a result of hypoglycaemia.
Glucagon is a well-known hormone that counters the action of insulin.
Tip: This article contains other tips on how to face a hypoglycemic episode.
Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHNS)
Hyperosmolar Hyperglycemic Nonketotic Syndrome is a rare condition; however, it is wise that you learn about it to help you handle it or that of your loved one if it occurs.
HHNS is more like the opposite of hypoglycemia. It is when your blood glucose level is abnormally high. It can lead to death.
It is wise that as a diabetic patient, you keep a close watch on your blood glucose level, especially when you are sick. This is one way to avoid HHNS because it would help you detect early enough when your blood sugar level starts to climb.
[et_bloom_locked optin_id=optin_3][/et_bloom_locked]
Gastroparesis
Prolonged high blood sugar level can as well cause damage to the vagus nerve.
Vagus nerve is the primary nerve that controls the movement of food through the gastrointestinal tract. Gastroparesis occurs when this nerve gets damaged, thus loses its function.
With damage to vagus nerve as a result of uncontrolled diabetes, there will be a delayed gastric emptying i.e the stomach takes longer time to empty its content.
Asides that, it could affect the management of blood glucose levels as you may not be able to effectively absorb food.
Other symptoms of gastroparesis include:
§ The feeling of fullness
§ bloating
§ nausea and vomiting
§ heartburn
§ loss of appetite
§ stomach spasms
One way to help manage this condition is by sticking to low fibre foods and avoiding high-fat foods. You may require to make considerable changes to your Diabetes-friendly Food and Diet.
Complications Timeline of Uncontrolled Type 2 Diabetes
As you know, diabetes mellitus is one of the most common chronic health conditions. This means it takes its time and can extend over a long period of time.
In cases where it is well managed, it may not interfere much with the persons’ normal life. However, it doesn’t erase the fact that such person is still at risk of the complications I mentioned above.
First 10 Years From the Diagnosis of Diabetes (Type 2)
Most people with type 2 diabetes are usually not aware of it for some time. For this reason, some organ damage may even be present at the time of diagnosis.
Here are some features indicating other issues that may be present with diabetes at the type 2 diagnosis.
§ A high blood glucose level
§ Peripheral neuropathy
§ Microalbuminuria
The person at this point should start with urine screening exams, foot exams as well as retinal exams.
After 10 Years of Diagnosis
Complications at this point usually arise from genitourinary organs.
For example, 50% of diabetic men who do not manage their health condition present with erectile dysfunction at this point.
After 20 Years of Diagnosis
At this stage, the kidney is much likely to be affected in an uncontrolled case of diabetes type 2.
For one that has developed nephropathy before now, it could advance to the end-stage renal disease at this point.
You should note that depending on how well you manage your condition, nephropathy and cardiovascular issues could occur at any point in time.
Due to the array of complications that are associated with diabetes type 2, life expectancy for those that poorly control theirs is usually 7 to 10 years shorter than that of those who are not diabetic or those who are well-managed diabetes.
Remember, if you have a senior battling with type 2 diabetes mellitus, ensure that they get the appropriate medical care and attention because asides their health condition, their age is also a predisposing factor to other ailments. So, sometimes, you cannot blame just ‘diabetes’.