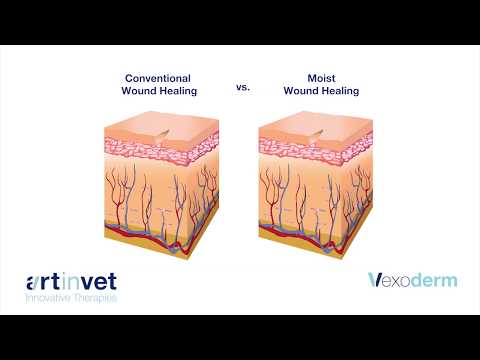
Over the years, the approach to wound healing has been exclusive just to restore the normal state of the epidermis and restore balance. This was mainly done using a dry wound healing approach. However, there is more to wound healing in recent times with the discovery of the importance of creating a moist wound healing environment.
This article will tell you what moist wound healing is and how it will benefit the elderly. Most importantly, the best moist wound healing options for seniors and the elderly.
Today, very good care is not optional when dressing wounds in seniors because those wounds are ‘fragile’.
Before jumping on to the best moist wound healing options for seniors, let’s find out what moist wound healing really is…
What is Moist Wound Healing?
Moist wound healing is a process whereby wound healing takes place in a moist environment. The moist environment comprises the area around the wound bed.
By treating wounds in a controlled wet environment, the delivery of antimicrobials, analgesics, and other bioactive molecules such as growth factors and micrografts become more efficient.
Indications for Moist Wound Healing
Different wounds require different healing options. Some wound conditions determine the type of wound dressing to use.
Here are some moist dressings and their indications
- Alginate dressing
The indication for Alginate dressing includes;
# For primary treatment in moderately to heavily exuding partial-thickness wound.
An example of this type of wound is stage 2 pressure ulcers.
# Alginate dressings are also indicated for use in full-thickness wounds like stage 3-4 pressure ulcers, dermal wounds, surgical wounds, dehisced wounds, tunneling wounds, sinus tracts, and donor sites.
# They can also be used in infected wounds and post-operative wounds with minimal bleeding.
- Collagen dressing
The indication for collagen dressing include:
# As a primary dressing in the treatment of partial and full-thickness wounds such as skin grafts, donor sites, surgical wounds, tunneling wounds, infected and non-infected wounds.
# You can also use them for wounds with minimal to heavy exudates.
- Antimicrobial dressing
The indications for antimicrobial dressing includes:
# As a primary or secondary dressing in the treatment of draining, exuding, infected and non-healing wounds.
# The antimicrobial dressing will help to protect different categories of wounds from bacterial infection.
- Composite dressing
The indications for composite dressings include:
# As primary treatment of small to heavily draining, partial- and full-thickness wounds like stage 2-4 pressure ulcers, dermal ulcers and surgical incisions.
- Contact layer dressing
This can be used as a primary dressing on partial and full-thickness wounds with minimal to heavy exudates, donor sites and split-thickness skin grafts.
- Foam dressing
You can use this for primary and secondary dressing for small to heavily exuding partial-thickness wounds and full-thickness wounds like stage 2-4 pressure ulcers, surgical wounds, and dermal ulcers.
You can also use it on infected wounds, tunneling wounds, or cavity wounds. However, it is highly dependent on the product.
Foam dressings also protect against friction.
- Hydrocolloid dressing
Indications for Hydrocolloid dressing includes:
They are indicated for use either as a primary or secondary dressing in the treatment of lightly to moderately exuding partial and full-thickness wounds like dermal ulcers, venous ulcers, skin tears, lacerations, pressure injuries, or wounds.
- Hydrogel dressing
Hydrogel dressings can be used in the treatment of stage 2-4 pressure ulcers, deep wounds, minor burns, infected wounds, dermal ulcers, skin tears, donor sites, radiation dermatitis, etc.
- Medical grade honey dressings
The indication for this dressing include:
# On partial and full-thickness wounds
# acute or chronic wounds such as venous insufficiency ulcers, stage 2-4 pressure ulcers, foot ulcers
# For first and second-degree burns, donor sites, traumatic wounds, surgical wounds.
# For fungating wounds, superficial wounds, and
# For wounds with bad odor.
- Silicone gel sheets dressing
You can use silicone gel dressing to prevent or improve the appearance of old and new hypertrophic and keloid scars.
- Specialty absorptive and super absorbent dressings
They can be used as the primary or secondary dressing in managing surgical incisions, lacerations, abrasions, burns, donor, or skin graft sites.
- Wound filler dressing
Filler dressings can be used as a primary dressing to treat minimally to moderately exuding partial and full-thickness, infected, and deep wounds requiring packing to fill dead space.
- Cloth dressings
This is most suitable for minor injuries like grazes, cuts or areas of delicate skin.
How Long Should You Keep a Wound Moist?
Most people adopt the general approach of treating a minor wound. This approach is, clean up the wound, stop the bleeding and expose it to air. This approach over time has been believed to speed up the healing process and also prevent infection.
However, recent research suggests that this approach is not ‘ideal’ because exposing wounds to air creates a dry environment that promotes cell death.
Tip: It is not the best practice to use hydrogen peroxide to clean wounds. Don’t do it!
When wounds are kept moist and covered, blood vessels regenerate faster. Not only that, the number of cells that could cause inflammation drop more rapidly than they do in wounds opened to air out.
Therefore, the best would healing approach is to keep a wound moist and covered for at least 5 days.
The Best Moist Wound Healing Options For Seniors
Now let’s turn on to the best moist wound options for seniors. Remember, seniors have delicate skin, so your approach to would healing should be delicate too.
Let’s look at the options one by one…
- Low adherent dressing
The low adherent dressing has a major characteristic of allowing exudate to pass through into a secondary dressing while maintaining a moist wound bed.
They are also quite cheap and easy to find.
These dressings are manufactured in the form of tulles, which are open weave cloth soaked in soft paraffin or chlorhexidine, textiles or multilayered films.
This dressing is made to help reduce adherence at the wound bed, and they are most suitable for patients with sensitive skin.
Most injuries in seniors have sticks or become adherent to the bed. So, using of this low adherent dressing will be very much suitable and also convenient.
- Semipermeable films
The mechanism of action of the semipermeable film is to accelerate wound healing by being permeable to air and water vapor and impermeable to fluids and bacteria. Their control is dependent on the moisture and transmission rate.
They are highly flexible and suitable for wounds that occur on difficult anatomical sites, such as those that occur over joints.
This is suitable for seniors because they already have other complicating health issues to deal with. So, adding bacteria infection will cause more harm.
It is best for your health care professional to decide the suitability of the semipermeable film options to your specific wound.
In other words, a careful assessment is needed because of the downside of this dressing. The downside is that they can’t hold a large amount of exudate. This can cause maceration of the skin which surrounds the wound bed.
These semipermeable films are among the major recent advances in wound management. They contain a sterile plastic sheet of polyurethane coated with hypoallergenic acrylic adhesive and are also used as a transparent primary wound cover.
- Hydrocolloids
These Hydrocolloids are used to rehydrate dry necrotic eschar and they promote autolytic debridement. They are impermeable to water vapor and air, unlike semipermeable films.
Also, they reduce wound pain. Because of their barrier property, the patients can shower and carry on with their normal activity without fear of infection.
If Hydrocolloids are used on wounds that require frequent inspection, like foot ulcers, care should be taken.
Your loved one needs is to be as comfortable as possible, not minding the type of wound dressing used. This particular Hydrocolloid has added advantage because it helps in the reduction of wound pain.
It is also comfortable because patients can carry on their normal activities like showering. This will bring as much comfort as possible and save you additional stress as a caregiver.
- Hydrocolloids with hydro fibers
Hydrocolloid fibers can be found in the form of a hydrophilic, non-woven flat sheet, referred to as hydro fiber dressings.
When they come in contact with exudate, fibers will be converted from a soft coherent gel sheet. This makes Hydrocolloids ideal for a large amount of exudate.
Suppose your loved one has wounds that bring out a late amount of exudate. In that case, Hydrocolloid with hydro fibers will be the best alternative.
No matter how much you love the senior in question, having to clean the late exudate coming out from the wound constantly will definitely irritate you. Therefore, using this particular Hydrocolloid saves you from that burden as it largely absorbs exudates.
- Hydrogel
The content of Hydrogel includes a matrix of insoluble polymers with up to 96% water content. This enables them to donate water molecules to the wound surface and maintain a moist environment at the wound bed.
Hydrogels can absorb a degree of wound exudate because the polymers are only partially hydrated. The amounts of exudates various Hydrogels absorb vary with brands. They can transmit vapor and oxygen. They are also permeable to bacteria, but their permeability is highly dependent on the type of secondary dressing used.
Hydrogels help promote wound debridement. The mechanism of action is by rehydration of non-viable tissue which helps in facilitating the process of natural autolysis.
Amongst all the Hydrogels, amorphous Hydrogels are the most commonly used. They are thick, viscous gels.
Hydrogels are best suited for sloughy or necrotic wounds.
This dressing is also the best for your loved one if the wound contains a high exudate.
- Alginates
They are two categories of Alginates.
# Alginates with 100% calcium and
# Alginates with a combination of calcium with sodium Alginate, usually in the ratio of 80:20.
They are made from naturally occurring calcium and sodium salts of alginic acid found in the family of brown seaweed.
The acid content of Alginates is mannuronic acid and glucuronic acid. The amount of each acid contained determines the amount of exudate absorbed and the shape of dressing it will retain.
Once Alginates come in contact with wound fluid, it dissolves to form a hydrophilic gel. This is a result of the exchange of sodium ions in wound fluid to form a hydrophilic gel.
Alginates that are high in mannuronic acid can be washed off the wound easily with saline, whereas those in guluronic acid retain their basic structure therefore, they need to be removed from the wound bed in one piece.
Alginates can absorb 15 to 20 times their fluid weight, which will make them highly suitable for exuding wounds.
- Foam dressings
They function to transmit moisture vapor and oxygen and also provide thermal insulation to wound beds. These foam dressings are either manufactured as polyurethane or silicone foam.
Polyurethane foams are highly absorbent because they consist of 3 layers. These three layers include a hydrophilic wound contact surface and a hydrophilic backing. These layers facilitate iodine low uniform dispersion of exudates throughout the absorbent layer and also prevent exterior leakage.
Silicone foams consist of a polymer of silicone elastomer, which is derived from two liquids. When the two liquids are mixed, they will form a foam while expanding to fit the wound shape forming a soft open-cell foam dressing. Silicone foam dressing also protects the area around the wound from further damage.
Generally, the most striking advantage of foam dressings is their ability to contain exudate.
- Antimicrobial dressing
Silver and iodine have been majorly used as antimicrobial dressings. Silver has been widely used in the treatment of burns in its ionic or nanocrystalline form.
Iodine can lower microbial load in chronic wounds. As fluid is absorbed, iodine is released slowly, which will lead to reducing the bacteria load and debridement of the wound debris.
Due to this mechanism of action, iodine is deposited over a long period, leading to the maintenance of the constant level of iodine in the wound bed.
However, suppose a patient has thyroid disease. In that case, caution should be taken because they might be a systemic uptake of iodine. In a situation where the treatment has to continue, thyroid function should be regularly monitored.
Benefits of Moist Wound Healing Dressing
Dressings were primarily used to absorb fluid, protect the wound from injury, and also limit its exposure to infections. It was originally believed that scabs formed from the normal dressing were part of the healing process; however recent discoveries showed that it is not so. Moist wound healing not only prevent scab, but it also facilitates the healing process.
Some of the benefits of moist wound healing include the below.
1. It takes less time to heal
In a moist wound healing environment, the body focuses all its attention on healing the wound rather than protecting it. This is not so for normal-dry wound healing because the body creates scabs that require time and energy in dry healing.
Also, wet wound healing use energy to break down the scab after the wound is healed.
2. Moist wound healing improves the function of keratinocyte cells
Keratinocytes have a critical role in wound healing, and it is a major component of the epidermis.
Keratinocytes has a very strong connection with other cells that are involved in wound healing. This relationship is very important for wound healing.
In cases of dry wounds, keratinocytes will have to find their way underneath the wound bed to find a moist area that will enable it to move forward.
However, in a moist wound healing environment, keratinocytes can easily travel across the wound surface.
3. Moist wound healing facilitates autolytic debridement
Wounds contain endogenous proteolytic enzymes that are trapped in a moist environment. Trapping the enzymes enables them to perform autolytic debridement more efficiently, and this helps them to break down necrotic (dead) tissue.
In addition to speeding up the healing process, moist wound environments allow for the body’s natural healing process to work more effectively.
4. Moist wound healing reduce the chance of wound infection
In a hypoxic environment, wounds are rarely infected. Moist wound healing environment reduces the chances of infected wounds by creating a hypoxic environment in the wound bed.
This will promote angiogenesis, decrease the pH. and make the wound area not habitable to bacteria.
5. Moist wound healing preserves the growth factors in wound fluid
During tissue repair, growth factors are needed. Growth factors are natural proteins that control key cellular activities during the tissue repair process. Moist wound healing will allow the growth factor to be preserved on the wound bed, and it will help tissues to be repaired quickly.
6. Moist wound healing stimulates the synthesis of collagen
Collagen forms the basis for the formation of new tissue, which will facilitate the healing process. The increased production of this collagen helps the body lay down the matrix for new tissue, thereby attracting the cells necessary for healing.
7. Moist wound healing reduces pain
Moist wound helps in reducing pain. When the pain is reduced, there will be a reduction in stress response and also less fatigue in patients. This will aid improvement in the healing process.
When the pain is less, the patient will be better able to help themselves in terms of mobility.
8. Moist wound healing reduces scarring
The process of moist wound healing treatment promotes the growth and movement of new cells. Also, it ensures that proteins needed for closing the wound are efficient. This will lead to reduced inflammation and also promotes more even skin formation.
What Does Research Say?
According to research carried out by Johan P.E. Junker, Rami A. Kamel, and Elof Eriksson, successful treatment of wounds is greatly dependent on the precise control and continuous monitoring of the wound-healing process. It has been observed that wet or moist treatment of wounds promotes re-epithelization and result in scar formation.
The modern concept is to treat wounds in a controlled wet environment, which deliver antimicrobials, analgesics, other bioactive molecules such as growth factors.
Although several manufacturers produce moist wound healing products and try to implement the concept, there is still a lack of commercial translation of wet wound healing principles into clinically available products.
In research, the moist environment was shown to improve the healing process of the wound, preventing dehydration and enhancing angiogenesis and collagen synthesis together with increased breakdown of dead tissue and fibrin. When this is done, the aesthetics of the wound, and lead to decreased pain.
This mechanism causes the wound to heal fast in a moist environment, but some factors drive that. This could be due to
- easier migration of epidermal cells on a moist surface,
- faster epithelization, and also
- prolonged presence of proteinases and growth factors.
Also, clinical studies have observed that wound fluid from wound healing under moist conditions stimulates keratinocytes proliferation and fibroblast growth with subsequent preservation of growth factors for wound repair.
Moreover, wounds that were allowed to heal in a moist environment were vascularized at a greater rate than those maintained under dry conditions. Also, for moist wounds, angiogenesis occurred in a more orderly fashion.
What Are The Limitations of Moist Wound Healing?
Like everything else, there are some limitations of the moist wound healing method too.
Let’s explore them now…
1. Excessive moisture
Moisture is essential for wound healing, but it becomes harmful when it is excessive.
Wounds usually produce fluid that is rich in protein-melting enzymes. These enzymes will help to remove dead tissue from the wound bed.
If enzymes can melt protein, they also tend to melt the normal skin around the wound. Also, when the wound is excessively wet, it can promote yeast and fungus growth.
When the excessive wound becomes the issue, you can use protectants like zinc oxide, petroleum jelly, dimethicone, or film-forming skin barriers like skin prep.
2. Swelling
Blood and oxygen are essential for wound healing. Blood serves to provide protein and nutrition that will help in building new tissue, while oxygen helps in keeping the tissue alive.
When there is swelling, it means that there is excessive water in between the cells.
This extra water displaces the small blood vessels that will supply blood and oxygen. This will make wound healing very difficult.
3. Presence of yeast or fungus
When there is too much yeast or fungus in the wound, it will keep the wound wet, warm, and dark. This creates a perfect environment for the yeast and fungus to keep growing.
4. Formation of biofilms
Germs usually form a slimy colony on the wound surface called biofilm. Germs produce different chemicals and operate cooperatively. They protect each other by sharing antibiotic-resistant genes.
Conclusion
Moist wound healing is very beneficial for wounds to speed up recovery. There are cases where other types of healing are highly recommended, but moist wound healing is generally most recommended.
Always discuss with your health care personnel in cases of severe wounds to advise you on the best healing approach to use. Especially when you use most wound healing options for seniors.